Holistic Recovery from Operational Stress: Championing a new approach to post-traumatic growth for firefighters, leading to faster recovery and return to duty
In 2022, Fire Captain Mike Sears faced significant stress and health issues, leading him to take a leave of absence and attend the BC firefighter resiliency program. There, he learned new communication and self-care strategies. After returning to work, he applied these techniques during a traumatic call involving a high-speed car accident.
Mike introduced a non-traditional peer support method, encouraging crew members to express their emotions rather than just recounting details. This approach helped them process the difficult event they witnessed and maintain family connections.
Mike emphasized the importance of evolving communication practices to support both personal and professional relationships, highlighting the need to address and process traumatic experiences to prevent compounding emotional injuries and maintain relationships.
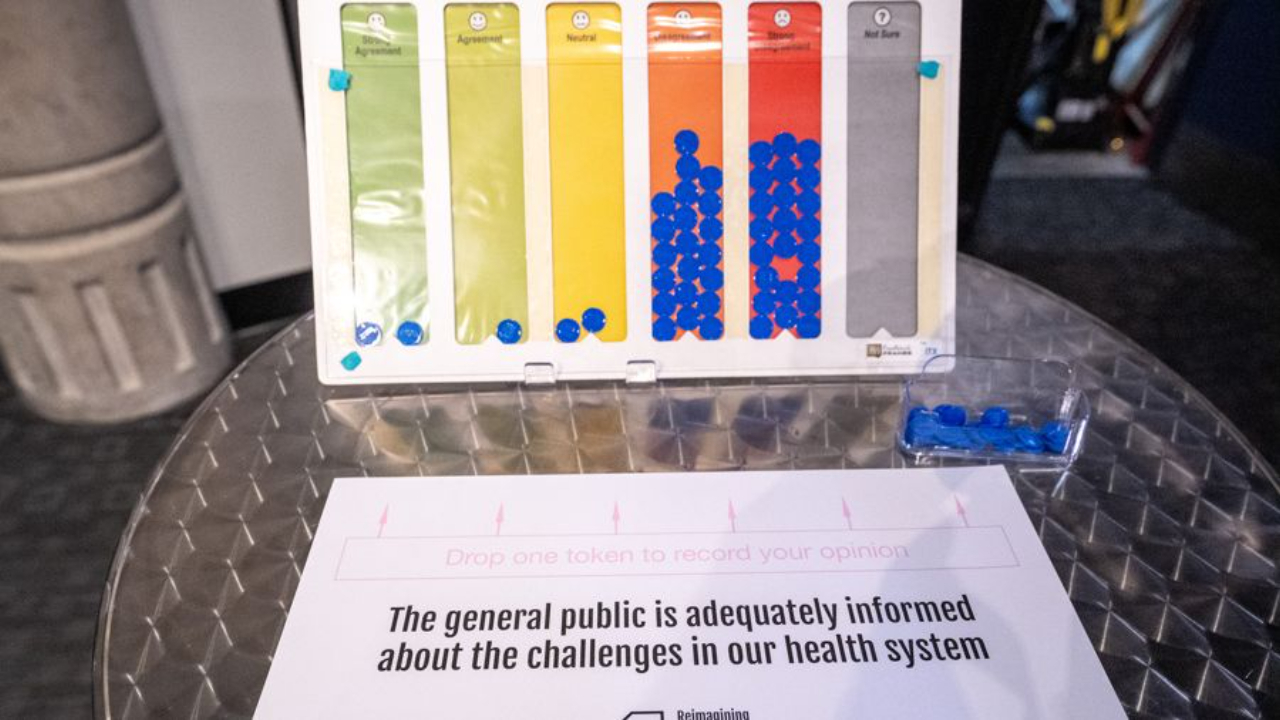
How Well Does the Public Understand the Challenges in Our Health Care System?
Picture this: You're standing at a podium during your hospital's annual community meeting. The room is packed with engaged citizens, local media, and community leaders. You're explaining the complex reasons behind emergency department wait times, but as you scan the room, you see furrowed brows and skeptical expressions. Despite your clear explanation, there's a palpable disconnect between your understanding of the challenges and how your audience perceives them.
If this scenario feels familiar, you're experiencing a phenomenon that's becoming increasingly common across Canadian health care leadership. And it's not just your imagination – the data tells a compelling story about this growing disconnect between health care leaders and the public we serve.
In our poll at Reimagining Health Care Leadership, 83.9% either disagreed (38.7%) or strongly disagreed (45.2%) with the following statement, “The general public is adequately informed about the challenges in our health system.”
T...
Taking a Thoughtful Pause Before Leaping into Action: Applying Theory U in Health Care Leadership

If you're a health care leader reading this, you're probably thinking, "Thoughtful pause? In my organization? Have you seen my schedule?" Whether you're leading a hospital, directing a school for future health care professionals, or heading a regulatory college, the pressure to act quickly is constant and intense.
The health care sector moves at lightning speed. Patient lives, student futures, and professional standards hang in the balance. Quick decisions are often necessary. But here's a thought: what if taking strategic pauses could actually help you move faster in the right direction?
The Challenge
The resistance to pausing in health care settings is real and understandable. Here's what you're up against:
- Deeply ingrained professional training that emphasizes rapid response
- Resource constraints that create constant time pressure
- Complex regulatory requirements demanding quick decisions
- A culture that often equates speed with competence
- The fear that pausing might ...
Designing Health Care Spaces that Heal: Creating uplifting, human-centered health care environments that promote dignity, optimism, and wellness
In this video from our Reimagining Health Care Leadership event, architect Vincent Van den Brink shares how a personal experience with his mother, who was undergoing cancer treatment, inspired him to rethink design at his firm, Break House.
He emphasizes the importance of human-centric design, focusing on user experiences rather than aesthetics. This shift made him prioritize patient comfort and emotional well-being in his work. He highlighted key insights from patient surveys, such as the need for natural light, privacy, and a connection to nature. This approach has since been applied to projects like a large undertaking for Shannex, where they aim to enhance the quality of life for seniors by designing spaces that cater to their needs and experiences.
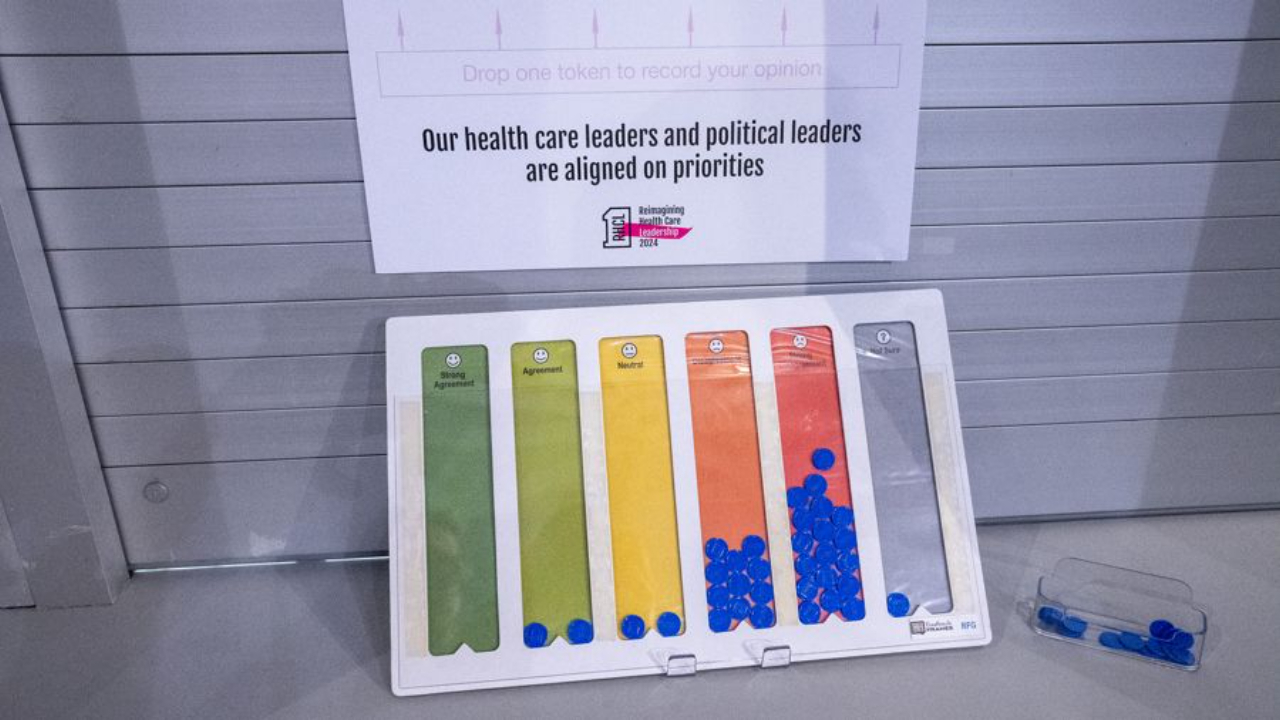
Is There Alignment Between Health Care and Political Leaders on Priorities?
As a leader of a Canadian health care organization, you understand the importance of having a clear strategic direction that allows you to deliver quality care to your patients and communities, educate future health professionals, or create and maintain policies and procedures to protect the public. You've collaborated with your teams, analyzed trends, and set evidence-informed priorities to guide your decision making. You feel confident that you're steering your organization in the right direction.
But then the political winds change. Suddenly, the priorities you've carefully established seem misaligned with the new focus coming from your provincial capital or Ottawa. Projects you've invested in get stalled or discontinued. Funding shifts toward initiatives that, while flashy, don't address the most pressing needs of patients, students, or practictioners.
The troubling reality is that health care and political leaders are often dramatically misaligned on priorities:
When we polle...
Leveraging Physical Spaces to Transform Relationships in Health Care

As a health care leader, you're probably rolling your eyes at yet another article about organizational change. Between managing clinical excellence, navigating regulatory requirements, and keeping the lights on, who has time to think about furniture arrangements and office layouts? I get it. Whether you're leading a hospital, running a regulatory college, or directing a professional association, your plate isn't just full - it's overflowing.
But here's the thing: environmental design might be one of the most underutilized tools in your leadership toolkit. And if you're wondering why that matters when you're dealing with staffing shortages and budget constraints, stick with me for the next few minutes.
Why This Is Harder Than It Looks
The challenges you're facing aren't small:
- Clinical spaces are often designed for efficiency and patient care, not relationship building - and changing them requires navigating complex approval processes and regulatory requirements
- Professional...
The Power of Permission in Leadership: The impact of giving yourself permission to succeed, fail, and show up fully in both life and work
In this video from our Reimagining Health Care Leadership event, Nikki Martin, DE&I Consultant and Inclusive Leadership Trainer and one of our strategic planning colleagues at OnePagePlans shares her journey as a person of color, highlighting her interracial upbringing and the impact of her parents' ‘revolutionary’ marriage.
She discusses the challenges of growing up biracial, feeling marginalized, and the struggle to find her identity. Nikki’s turning point came in 2020 during the lockdown, when she co-founded the Black Wellness Cooperative (BWC) with other black fitness professionals. The BWC provided a supportive community, leading to her realization of the importance of self-care and the permission to be exceptional.
She emphasizes the need for authentic leadership and advocating for spaces where individuals can be their full selves and lead with vulnerability and bravery.
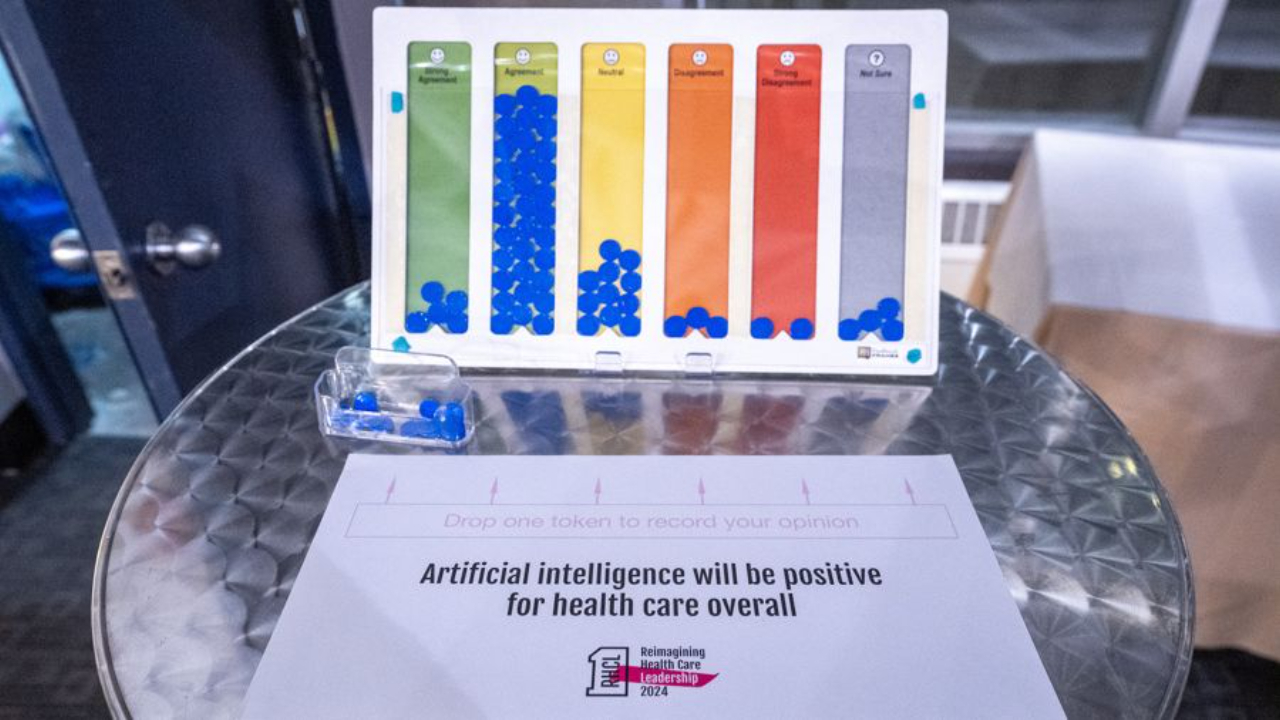
AI in Canadian Health Care: Leading Through (another!) Digital Revolution
As a health care leader, you're likely hearing about artificial intelligence (AI) constantly. Your clinicians, staff, or faculty probably share articles about its potential to transform their work – some with excitement, others with extreme trepidation. Your board might be asking about AI strategy while your IT team warns about infrastructure gaps. And somewhere in between, you're trying to chart a course that serves your patients, your public, or your students while supporting your internal team and maintaining financial sustainability.
For a technology that is supposed to make things easier, the conversation around AI seems to be incredibly complex and overwhelming.
At our Reimagining Health Care Leadership event, we polled the audience on the statement, “Artificial intelligence will be positive for health care overall.” The results were not as conclusive as many of our other poll questions:
- Strong Agreement: 9.1%
- Agreement: 45.5%
- Neutral: 24.2%
- Disagreement: 12.1%
- Strong Di...
Beyond Small Talk: Building Authentic Dialogue and Supporting Well-being in Health Care Leadership
As a health care leader, you know the weight of responsibility that comes with guiding organizations through complex challenges while supporting your colleagues' well-being. Whether you're leading a teaching hospital, running a regulatory college, or directing a professional association, you're likely feeling the tension between maintaining operational excellence and creating space for authentic dialogue about well-being.
The pressures of health care leadership can make deep, meaningful conversations feel like something that you have neither the time nor the headspace for. But what if I told you that the quality of your conversations could be the key to both organizational success and your team’s well-being?
The Leadership Challenge: Why Authentic Dialogue is Hard in Health Care
The obstacles to authentic dialogue in health care settings are real and significant.
Here's what I've observed while working with health care leaders across Canada:
- Time constraints create a default...
Housing as a Key to Health: How diverse housing options improve well-being and health outcomes for communities
In this video from our Reimagining Health Care Leadership event, Marie-France LeBlanc, CEO of the North End Community Health Centre, discusses the transformation of a Travelodge motel into the Overlook, a residence for 60 chronically homeless individuals battling mental health and addiction issues.
NECHC's approach emphasizes housing as a foundation for health, offering wraparound services, community, and dignity. Marie-France also discusses a police incident at the Overlook that underscored the lack of value placed on such communities.
She advocates for housing as a health intervention essential for individual and societal health and calls for systemic change to prioritize housing as a basic human right.

